Antibiotics are commonplace — used to treat minor and major infections, prevent infection post-surgery, and treat our pets and livestock.
But what happens if these life-saving drugs lose their efficacy?
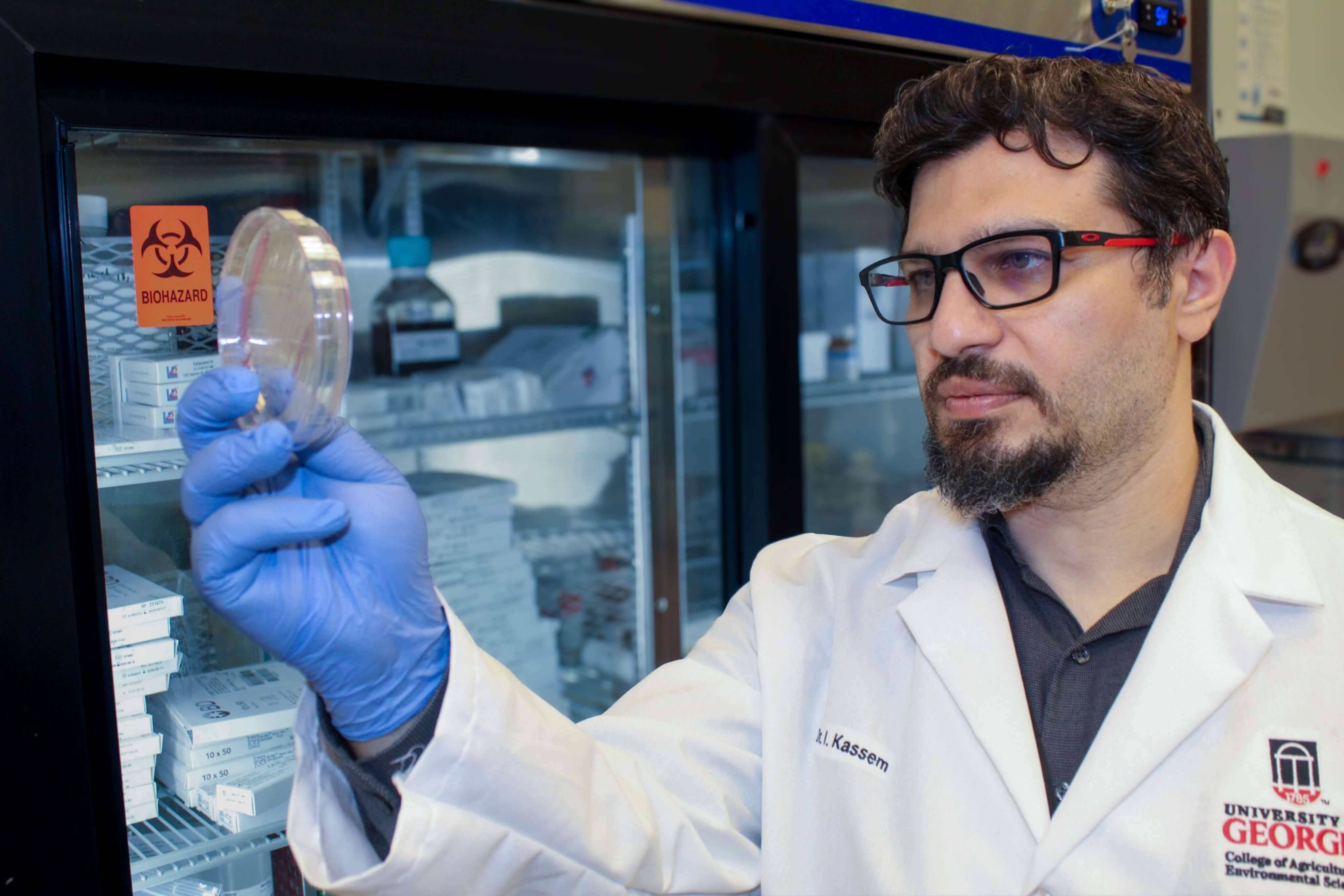
Issmat Kassem, assistant professor at the University of Georgia College of Agricultural and Environmental Sciences, has asked this question for nearly two decades.
“Antimicrobial resistance is one of the 10 major issues facing humanity, not only for humans but other animal populations — both livestock and pets,” said Kassem, who serves as faculty within the UGA Center for Food Safety. “Antimicrobial resistance was the third-leading underlying cause of death in 2019. The economic impact will also be huge, and humanity will suffer. We are talking about threatening human medicine as we know it.”
A new study from Kassem and his research team revealed that mobilized colistin resistance (MCR) genes were detected not only in sewage samples in Georgia, but also in bodies of freshwater post-treatment.
Colistin, frequently considered a last-resort antibiotic for treating difficult infections, is considered by the World Health Organization to be a critically important drug for treating human populations and of the highest priority. This means that colistin might be the only option to treat certain infections, and if it fails, the outcome can be devastating or even deadly for a patient.
In a follow-up to Kassem’s 2022 study, which discovered that a gene that causes antimicrobial resistance in bacteria is present in Georgia, the research team expanded the number of wastewater treatment plants monitored and tested nearby areas that received treated water.
“If something is happening that allows bacteria to survive colistin and if that gene or DNA material can jump between bacteria, the use of colistin will be jeopardized, resulting in the loss of an important tool in fighting infectious diseases,” Kassem said.
Wastewater analysis reveals antimicrobial resistance circulating in a community
All sewage generated by humans goes to a treatment plant, where solids and pathogens are removed before the water goes on to the environment. Raw, or untreated, sewage is a perfect matrix to see what is happening in a given population, according to Kassem.
Monitoring sewage provides comprehensive insights into the different infectious agents and antimicrobial resistance markers that might be circulating in the human population. Kassem and his team used this knowledge to detect genes responsible for colistin resistance for the first time in Georgia and the U.S.
New study identifies MCR gene in U.S. bacteria, raising public health concerns
The new study conducted by Kassem’s team expands the research from one bacterium — Morganella morganii — to see whether MCR genes could be identified in other bacteria.
One bacterial species, Serratia nevei, which has been found to carry the transmissible gene in other global regions, was identified as a carrier for the first time in the U.S. Serratia species include opportunistic pathogens that can cause urinary tract infections, endocarditis and other diseases in humans, especially within elderly and immunocompromised communities.
Another concerning feature of the unique bacterium: It can be foodborne.
The findings have informed the next steps for Kassem’s research team. Could Serratia nevei contaminate the food supply? Or could the food supply be the source? Kassem’s team aims to investigate which foods may be carrying Serratia nevei and the associated MCR genes.
“In the U.S., we do a really good job of monitoring our food,” Kassem said. “One of the culprits we are thinking about being implicated might be certain imported foods.”
While imported food is tested for pathogens, it is not tested for antimicrobial resistance genes. As Kassem and his team have discovered, those genes can be carried on a non-pathogenic bacterium and can jump to a pathogenic one.
“This is a call to look deeper into the connections between finding these genes in the environment and in humans. We are not just talking about sewage plants anymore,” Kassem said. “Based on the evidence we have now, we can say it is circulating in the human population and that it can be considered to be in the environment.”
Critical next steps to combat global spread of antimicrobial resistance
Kassem calls for a multifaceted approach to combat the transmission of antimicrobial resistance genes within the U.S., including monitoring systems, legislation and, above all, education.
“We need to expand our monitoring system and not fall into assumptions. Whatever happens in country A, it will spread to country B,” Kassem said. “We cannot rest; we must do preemptive work to prevent these things from coming. It's easier said than done, but precautions can — and must — be put into place.”
A grant from the UGA Center for Food Safety supported this research. Additional CAES researchers include Jouman Hassan, Tongzhou Xu, David Mann, Malak A. Esseili and Xiangyu Deng.
Learn more about Kassem’s research into antimicrobial resistance at the IKassem Lab website.